Why Suboxone?
Suboxone (buprenorphine/naloxone) is a life-saving medication used to treat opioid use disorder (OUD). It works by reducing cravings and withdrawal symptoms while blocking the effects of other opioids. People on Suboxone are less likely to relapse, overdose, or experience hospitalization.
Why You Need to Be in Partial Withdrawal
To start Suboxone safely, your body must be in partial opioid withdrawal. If Suboxone is taken too soon—while full opioids like oxycodone, heroin, or fentanyl are still active in your system—it can cause precipitated withdrawal, a sudden and intense worsening of symptoms.
This happens because buprenorphine kicks off the stronger opioids from your receptors too quickly. Waiting until you're in mild to moderate withdrawal ensures a gentler transition and better results.
This happens because buprenorphine kicks off the stronger opioids from your receptors too quickly. Waiting until you're in mild to moderate withdrawal ensures a gentler transition and better results.
What Does Withdrawal Feel Like?
Most patients feel symptoms like:
- Anxiety or restlessness
- Sweating or chills
- Muscle aches and cramps
- Nausea or diarrhea
- Yawning or runny nose
It’s not easy—but most people feel dramatically better by Day 3, and we’ll support you the whole way.
Medications We Use to Help You Get Through your Suboxone Induction
We can prescribe medications to reduce your discomfort during induction, including:
- Ibuprofen or naproxen – for body aches and cramps
- Hydroxyzine – for anxiety and sleep
- Imodium (loperamide) – for diarrhea
- Clonidine – to reduce blood pressure spikes, chills, and restlessness
- Ondansetron or promethazine – for nausea
- Trazodone – for sleep if needed
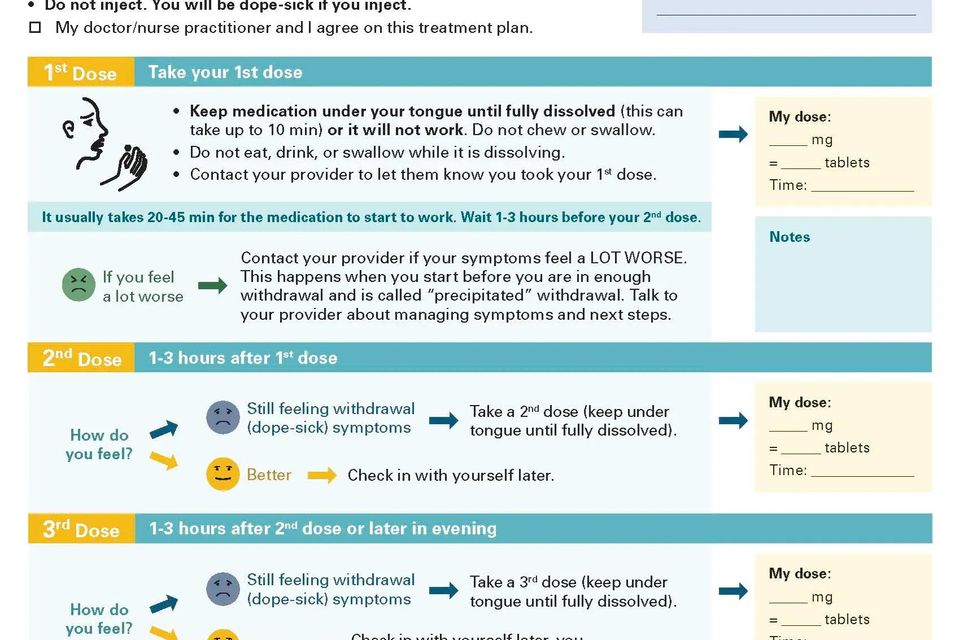
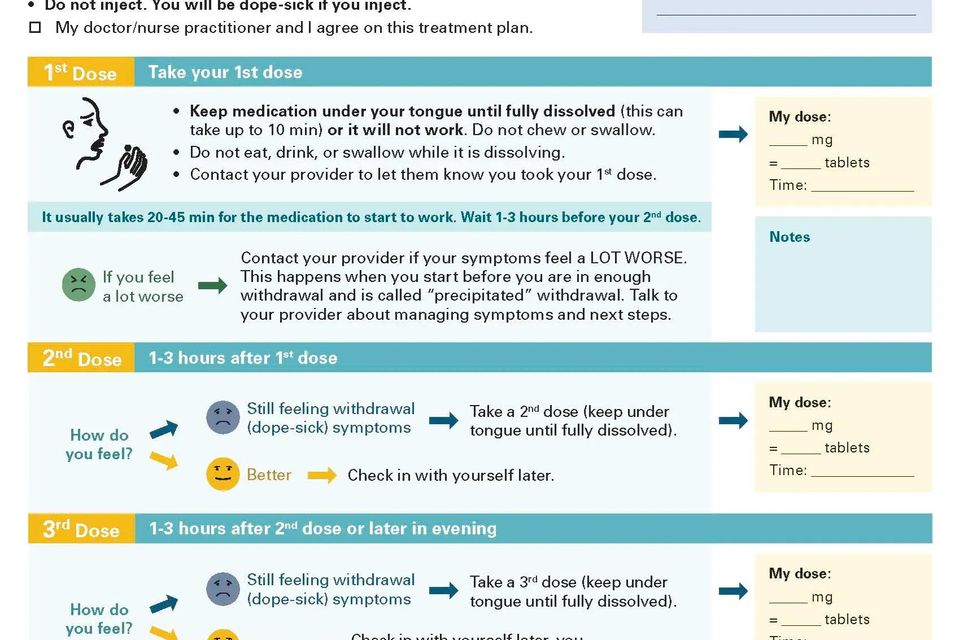
The Suboxone Induction Process
Here’s what to expect:
Day 1: Wait until you’re in partial withdrawal, COWS >12 (>17 optimal)
You’ll start to feel withdrawal symptoms 12–36 hours after your last opioid, depending on what you’ve been using. We’ll guide you in assessing when it’s the right time to begin.
Day 1–2: Start with a low dose
You’ll take a small test dose (typically 2 mg). If tolerated well, you can repeat doses every 1–2 hours until symptoms ease. The goal is to relieve withdrawal without overmedicating.
Day 3+: Maintenance
Most people feel significantly better by Day 3. We’ll check in regularly, adjust your dose if needed, and support your recovery plan—whether that includes counseling, therapy, or peer support.
Commitment & Safety
Suboxone works best when combined with regular follow-up and a willingness to work toward recovery. We ask that patients:
- Commit to follow-up appointments (usually monthly)
- Be honest about challenges and setbacks (no judgment)
- Understand the risks of combining Suboxone with alcohol or sedatives
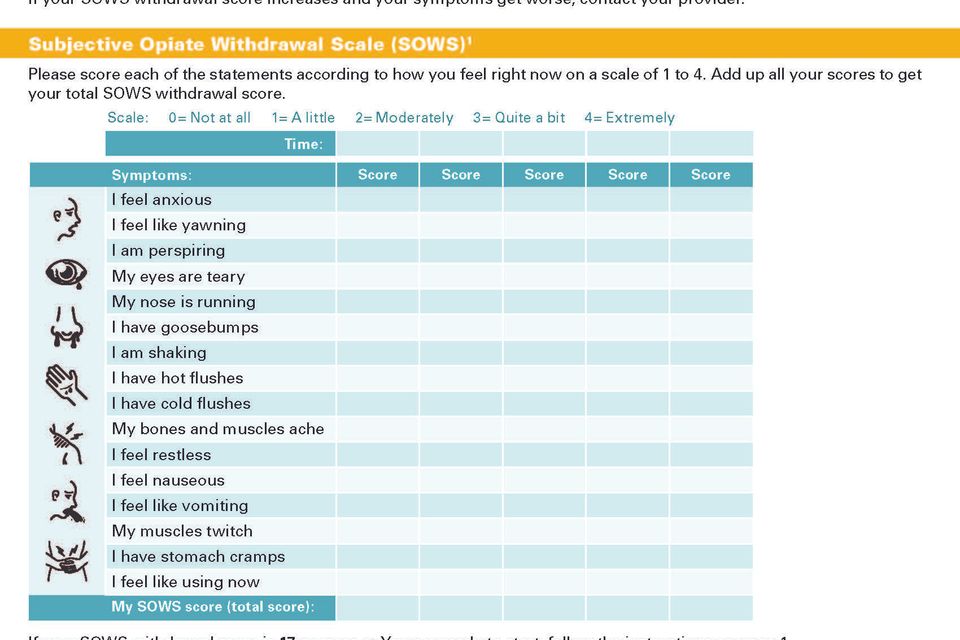
The Clinical Opiate Withdrawal Scale (COWS) is a tool we use to help decide when it's safe to start Suboxone.
Suboxone contains buprenorphine, which can cause precipitated withdrawal if taken too soon after using opioids. To avoid this, you need to be in moderate withdrawal—not just “feeling off.”
The COWS scale assigns points to common opioid withdrawal symptoms. A score of 12 or higher means you're likely ready to start Suboxone, with above 17 being optimal
Suboxone contains buprenorphine, which can cause precipitated withdrawal if taken too soon after using opioids. To avoid this, you need to be in moderate withdrawal—not just “feeling off.”
The COWS scale assigns points to common opioid withdrawal symptoms. A score of 12 or higher means you're likely ready to start Suboxone, with above 17 being optimal
Critical Safety Note: Loss of Tolerance = Overdose Risk
If you’ve been off opioids—even for a short time—your tolerance drops fast.
This can happen:
- After detox or rehab
- After being in jail or the hospital
- After simply trying to stop on your own
-
If you go back to using the same amount you used before, your risk of overdose skyrockets.
Suboxone protects you by giving your brain what it needs without the highs and chaos of full opioids. Staying on Suboxone dramatically reduces your risk of overdose or death.
Commitment, Safety & Overdose Prevention
Suboxone isn’t just a medication—it’s a foundation for recovery. At Be Well Berlin, we offer a judgment-free space to support your healing, but we also want you to understand what success looks like and how to stay safe along the way.
What We Ask of You:
To stay in care and get the most out of treatment, we ask patients to: - Commit to regular follow-ups
(Usually every 4 weeks, via telehealth unless otherwise indicated) - Be honest about setbacks or challenges
We won’t judge. Relapse can happen, and we’re here to help you get back on track—not punish you. - Avoid mixing Suboxone with other sedatives
Combining Suboxone with alcohol, benzodiazepines (like Xanax or Ativan), or other CNS depressants can increase the risk of overdose or sedation. - Have access to a blood pressure monitor and Narcan (naloxone)
We recommend checking your BP periodically, especially if taking medications like clonidine.
Narcan saves lives—it’s safe, free with most insurance, and can reverse an overdose in seconds.
Ask us for a prescription or where to get it.
Required Tools for Patients
To participate in treatment, we ask patients to have the following at home:
1. At-Home Urine Drug Tests (14-panel recommended)
We use drug screening to monitor your safety—not to punish. You can use:
- This CLIA-waived 14-panel test
Amazon Link → -
Alternatively, you may use an in-lab test (Quest/LabCorp) if preferred.
You’ll be asked to complete a test at your first visit, and periodically during treatment. You’ll send a photo of the results through our secure portal.
2. Blood Pressure Monitor
Especially helpful during induction or when using medications like clonidine, which can cause low BP.
Basic digital monitors are affordable and available at any pharmacy or online.
Basic digital monitors are affordable and available at any pharmacy or online.
3. Narcan (Naloxone)
- Even though Suboxone lowers overdose risk, Narcan is still essential—for you, a friend, or someone you love.
We can send a prescription to your pharmacy, or guide you to free access programs in your area.
Suboxone Treatment in California & Alaska — Covered by Insurance or Membership
Be Well Berlin provides discreet, compassionate Suboxone (buprenorphine-naloxone) treatment via telehealth across California and Alaska. Whether you’re in Anchorage, Mat-Su, Fairbanks, Juneau, Los Angeles, or San Diego, we make access to opioid use disorder (OUD) treatment simple and safe.
We are in-network with:
California:
- Medicare Part B
- Aetna (Medical & Behavioral)
- Cigna
- UnitedHealthcare
- Optum Behavioral Health
Alaska:
- Alaska Medicaid
- Aetna Behavioral Health
- Optum Behavioral Health
- Pending: Cigna, Moda Health
